 |
| Pelvic inflammatory disease |
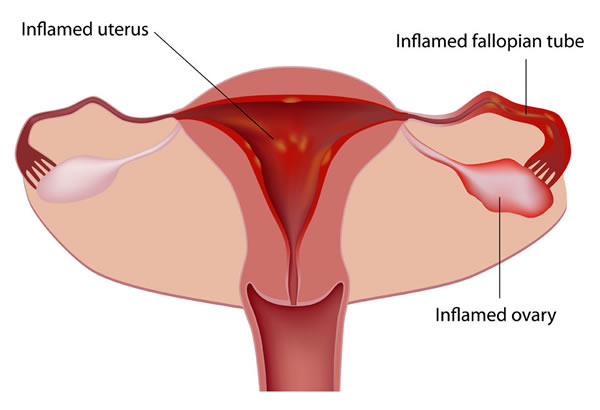
Pelvic inflammatory disease (PID) is a term used to describe any infection in the lower female reproductive tract that spreads upward to the upper female reproductive tract. The lower female genital tract consists of the vagina and the cervix. The upper female genital tract consists of the body of the uterus, the fallopian or uterine tubes, and the ovaries.
PID is the most common and the most serious consequence of infection with sexually transmitted diseases (STD) in women. Over one million cases of PID are diagnosed annually in the United States, and it is the most common cause for hospitalization of reproductive-age women.
Sexually active women aged 15–25 are at highest risk for developing PID. The disease can also occur, although less frequently, in women having monogamous sexual relationships. The most serious consequences of PID are increased risk of infertility and ectopic pregnancy.
  |
To understand PID, it is helpful to understand the basics of inflammation. Inflammation is the body’s response to disease-causing (pathogenic) microorganisms. The affected body part may swell due to accumulation of fluid in the tissue or may become reddened due to an excessive accumulation of blood.
A discharge (pus) may be produced that consists of white blood cells and dead tissue. Following inflammation, scar tissue may form by the proliferation of scar-forming cells (fibrosis). Adhesions of fibrous tissue form and cause organs or parts of organs to stick together.
PID may be used synonymously with the following terms:
- salpingitis (inflammation of the fallopian tubes)
- endometritis inflammation of the inside lining of the body of the uterus)
- tubo-ovarian abscesses (abscesses in the tubes and ovaries)
- pelvic peritonitis (inflammation inside of the abdominal cavity surrounding the female reproductive organs)
Causes and symptoms
A number of factors affect the risk of developing PID. They include:
- Age. The incidence of PID is very high in younger women and decreases as a woman ages.
- Race. The incidence of PID is 8–10 times higher in nonwhites than in whites.
- Socioeconomic status. The higher incidence of PID in women of lower socioeconomic status is due in part to a woman’s lack of education and awareness of health and disease, and due in part to barriers to her accessibility to medical care.
- Use and method of contraception. Induced abortion, use of an IUD, nonuse of such barrier contraceptives as condoms, and frequent douching are all associated with a higher risk of developing PID.
- Lifestyle. Such high-risk behaviors as drug and alcohol abuse; early age at first intercourse; a high number of sexual partners; and smoking all are associated with a higher risk of developing PID.
- Specific sexual practices. Intercourse during the menses and frequent intercourse may offer more opportunities for the admission of pathogenic organisms to the inside of the uterus.
- The presence of a sexually transmitted disease
. Sixty to seventy-five percent of PID cases are associated with STDs. A prior episode of PID increases the chances of developing subsequent infections.
The two major organisms that cause STDs are Neisseria gonorrhoeae and Chlamydia trachomatis. The main symptom of N. gonorrheae infection (gonorrhea) is a vaginal discharge of mucus and pus.
Sometimes bacteria from the colon normally in the vaginal cavity may travel upward to infect the upper female genital organs, facilitated by the infection with gonorrhea. Infections with C. trachomatis and other nongonoccal organisms are more likely to have mild or no symptoms.
Although PID is unusual in women who are not sexually active, disease organisms other than the gonococcus and C. trachomatis can occasionally gain entrance to the upper female reproductive tract and cause PID.
Cases have been reported from Canada, Norway, and South America of PID caused by pinworms, pneumococci, and Entamoeba histolytica, a pathogenic amoeba.
Normally the cervix produces mucus that acts as a barrier to prevent disease-causing microorganisms, called pathogens, from entering the uterus and moving upward to the tubes and ovaries. This barrier may be breached in two ways.
A sexually transmitted pathogen, usually a single organism, invades the lining cells, alters them, and gains entry. Another way for organisms to gain entry happens when trauma or alteration to the cervix occurs.
Childbirth, spontaneous or induced abortion, or use of an intrauterine contraceptive device (IUD) are all conditions that may alter or weaken the normal lining cells, making them susceptible to infection, usually by several organisms. During menstruation, the cervix widens and may allow pathogens entry into the uterine cavity.
Recent evidence suggests that bacterial vaginosis (BV), a bacterial infection of the vagina, may be associated with PID. BV results from the imbalance of normal organisms in the vagina— by douching, for example.
While the balance is altered, conditions then favor the overgrowth of anaerobic bacteria that thrive in the absence of free oxygen. A copious discharge is usually present. Should some trauma occur in the presence of anaerobic bacteria, such as menses, abortion, intercourse, or childbirth, these organisms may gain entrance to the upper genital organs.
The most common symptom of PID is pelvic pain. However, many women with PID have symptoms so mild that they may be unaware that they are infected.
In acute salpingitis, a common form of PID, swelling of the fallopian tubes may cause tenderness on physical examination. Fever may be present. Abscesses may develop in the tubes, ovaries, or in the surrounding pelvic cavity.
Infectious discharge may leak into the peritoneal cavity and cause peritonitis; or abscesses may rupture, causing a life-threatening surgical emergency.
Chronic salpingitis may follow an acute attack. Subsequent to inflammation, scarring and resulting adhesions may result in chronic pain and irregular menses. Due to blockage of the tubes by scar tissue, women with chronic salpingitis suffer a high risk of having an ectopic pregnancy.
An ectopic pregnancy develops when a fertilized ovum is unable to travel down the fallopian tube to the uterus and implants itself in the tube, on the ovary, or in the peritoneal cavity. This condition can also be a life-threatening surgical emergency.
IUDs
The use of intrauterine devices, or IUDs, has been strongly associated with the development of PID. Bacteria may be introduced to the uterine cavity while the IUD is being inserted or may travel up the tail of the IUD from the cervix into the uterus. Surrounding uterine tissue may show areas of inflammation, increasing its susceptibility to pathogens.
Some researchers, however, maintain that the connection between IUDs and PID has been exaggerated and that further research is necessary.
Susceptibility to STDs
Susceptibility to STDs involves many factors, some of which are not known. The ability of the organism to produce disease and the circumstances that place the organism in the right place at a time when a trauma or alteration to the lining cells has occurred are factors. The woman’s own immune response also helps to determine whether infection occurs.
Diagnosis
If PID is suspected, the physician will take a complete medical history and perform an internal pelvic examination. Other diseases that may cause pelvic pain, such as appendicitis and endometriosis, must be ruled out. If pelvic examination reveals tenderness or pain in that region, or tenderness on movement of the cervix, these are good physical signs that PID is present.
Specific diagnosis of PID is difficult to make because the upper pelvic organs are hard to reach for samplings. The physician may take samples directly from the cervix to identify the organisms that may be responsible for infection.
Two blood tests may help to establish the existence of an inflammatory process. A positive C-reactive protein (CRP) and an elevated erythrocyte sedimentation rate (ESR) indicate the presence of inflammation.
The physician may take fluid from the cavity surrounding the ovaries called the cul de sac; this fluid may be examined directly for bacteria or may be used for culture. Diagnosis of PID may also be done using a laparoscope, but laparoscopy is expensive, and it is an invasive procedure that carries some risk for the patient.
A newer diagnostic technique that has dramatically improved the accuracy of laboratory testing for PID and other STDs is the ligase chain reaction (LCR) technique. The LCR technique detects DNA from N. gonorrhoeae and C. trachomatis in a patient’s urine sample. LCR technology is less invasive as well as more accurate.
Treatment
Alternative therapy should be complementary to antibiotic therapy. Because of the potentially serious nature of this disease, a patient should first consult an allopathic physician to start antibiotic treatment for infections.
Traditional medicine is better equipped to quickly eradicate the infection, while alternative treatments can help the body fight the disease and relieve painful symptoms associated with PID. Some of the alternative treatments include diets, nutritional supplements, herbal remedies, homeopathy, acupressure, and acupuncture.
General recommendations
- Bed rest. Patients need to rest and reduce physical activity to help the body recuperate faster.
- Avoid sexual activity. Both patient and her partner should be treated for PID infections. They should also avoid sexual activity until their infections are completely eradicated.
- Healthy diet. Diet should include a variety of fresh fruits and vegetables. These foods contain high amount of phytonutrients and essential vitamins that help keep the body strong and stimulate the immune system to fight infections.
Nutritional supplements
The following nutritional supplements may be helpful:
- Daily vitamin and mineral supplements. These supplements can ensure that the body receives all the essential nutrients for normal body function. They also help keep the body strong to fight diseases including PID.
- Vitamin C. High-dose vitamin C (1–2 g) boost the immune function and help the body fight infection better.
Herbal treatment
The following herbal remedies may be helpful:
- Castor oil packs
. Patients can make warm packs by pouring castor oil on a clean piece of cloth wrapped in layers and warming it before placing on the lower part of their abdomen for up to 20 minutes. It is recommended that patients repeat this therapy every day for up to seven days.
- Echinacea spp., goldenseals and Calendula officinalis
. These herbs are believed to have antimicrobial activity and may be taken to augment the action of prescribed antibiotics.
- Grapefruit seed extract
. This herb has been used to fight a variety of infections including bacterial, viral, fungal, parasitic, and worm infections.
- Blue cohosh (Caulophyllum thalictroides)
and false unicorn root (Chamaelirium luteum)
. These remedies are recommended as tonics for the general well-being of the female genital tract.
Homeopathy
A homeopathic practitioner may prescribe a patientspecific remedy to help reduce some of the symptoms associated with PID. Herbs that are used in PID patients include Apis mellifica, Arsenicum album, Belladonna, Colocynthis, Magnesia phosphorica, and Mercurius vivus.
Acupressure
Acupressure (applying pressure on specific pressure points) can increase blood flow to the pelvic region, reduce pain, and promote general health.
Acupuncture
Acupuncture involves inserting needles at various points on the skin of the body. These needles are like antennae that direct qi (life force) to organs or functions of the body. This treatment may help with pain and also strengthen immunity. It is important that patients request disposable needles to prevent transmission of AIDS, hepatitis, and other infectious diseases.
Allopathic treatment
If acute salpingitis is suspected, treatment with antibiotics should begin immediately. The patient is usually treated with at least two broad-spectrum antibiotics that can kill both N. gonorrhoeae and C. trachomatis plus other types of bacteria that may have the potential to cause infection.
Hospitalization may be required to ensure compliance. Treatment for chronic PID may involve hysterectomy. Early treatment of suspected PID is essential because some strains of N. gonorrhoeae are showing increasing resistance to standard antibiotics as of 2002.
If a woman is diagnosed with PID, she should see that her sexual partner is also treated to prevent the possibility of reinfection.
Expected results
PID can be cured if the initial infection is treated immediately. If infection is not recognized, as frequently happens, the process of tissue destruction and scarring that results from inflammation of the tubes results in irreversible changes in the tube structure that cannot be restored to normal.
Subsequent bouts of PID increase a woman’s risk of complications. Thirty to forty percent of female infertility cases are due to acute salpingitis.
With modern antibiotic therapy, death from PID is almost nonexistent. In rare instances, death may occur from the rupture of tubo-ovarian abscesses and the resulting infection in the abdominal cavity. One recent study has linked infertility, a consequence of PID, with a higher risk of ovarian cancer.
Prevention
The prevention of PID is a direct result of the prevention and prompt recognition and treatment of STDs or of any suspected infection involving the female genital tract. The main symptom of infection is an abnormal discharge. To distinguish an abnormal discharge from the mild fluctuations of normal discharge associated with the menstrual cycle takes vigilance and self-awareness.
Sexually active women must be able to detect symptoms of lower genital tract disease. Frank dialogue regarding sexual history, risks for PID, and treatment options is necessary with a physician. Also, open discussions with sexual partners
Lifestyle changes should focus on preventing the transfer of organisms when the body’s delicate lining cells are unprotected or compromised. Barrier contraceptives, such as condoms
Women in monogamous relationships should use barrier contraceptives during menses and take their physician’s advice regarding intercourse