 |
| Pneumonia |
Pneumonia is an infection of the lung that can be caused by nearly any class of organism known to cause human infections. These include bacteria, amoebae, viruses, fungi, and parasites.
In the United States, pneumonia is the sixth most common disease leading to death; 2 million Americans develop pneumonia each year, and 40,000–70,000 die from it.
Pneumonia is also the most common fatal infection acquired by already hospitalized patients. In developing countries, pneumonia ties with diarrhea as the most common cause of death.
  |
Even in nonfatal cases, pneumonia is a significant economic burden on the health care system. One study estimates that people in the American workforce who develop pneumonia cost employers five times as much in health care as the average worker.
According to the Centers for Disease Control and Prevention (CDC), however, the number of deaths from pneumonia in the United States has declined slightly since 2001.
Description
Anatomy of the lung
To better understand pneumonia, it is important to understand the basic anatomic features of the respiratory system. The human respiratory system begins at the nose and mouth, where air is breathed in (inspired) and out (expired). The air tube extending from the nose is called the nasopharynx.
The tube carrying air breathed in through the mouth is called the oropharynx. The nasopharynx and the oropharynx merge into the larynx. The oropharynx also carries swallowed substances, including food, water, and salivary secretion that must pass into the esophagus and then the stomach.
The larynx is protected by a trap door called the epiglottis. The epiglottis prevents substances that have been swallowed, as well as substances that have been regurgitated (thrown up), from heading down into the larynx and toward the lungs.
A useful method of picturing the respiratory system is to imagine an upside-down tree. The larynx flows into the trachea, which is the tree trunk, and thus the broadest part of the respiratory tree.
The trachea divides into two tree limbs, the right and left bronchi. Each one of these branches off into multiple smaller bronchi, which course through the tissue of the lung.
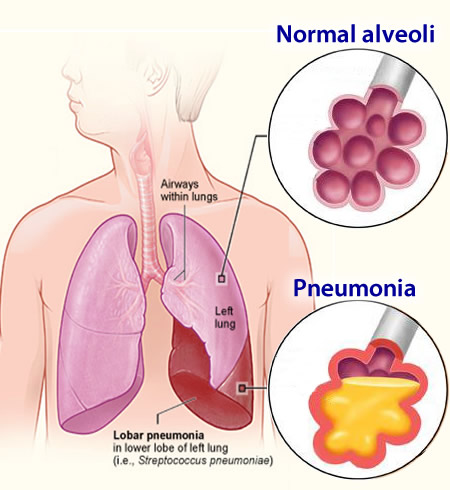
Each bronchus divides into tubes of smaller and smaller diameter, finally ending in the terminal bronchioles. The air sacs of the lung, in which oxygen-carbon dioxide exchange actually takes place, are clustered at the ends of the bronchioles like the leaves of a tree. They are called alveoli.
The tissue of the lung that serves only a supportive role for the bronchi, bronchioles, and alveoli is called the lung parenchyma.
Function of the respiratory system
The main function of the respiratory system is to provide oxygen, the most important energy source for the body’s cells. Inspired air (the air taken in when a person breathes) contains oxygen, and travels down the respiratory tree to the alveoli. The oxygen moves out of the alveoli and is sent into circulation throughout the body as part of the red blood cells.
The oxygen in the inspired air is exchanged within the alveoli for the waste product of human metabolism, carbon dioxide. The air you breathe out contains the gas called carbon dioxide. This gas leaves the alveoli during expiration. To restate this exchange of gases simply, you breathe in oxygen, you breathe out carbon dioxide
Respiratory system defenses
The healthy human lung is sterile. There are normally no resident bacteria or viruses (unlike the upper respiratory system and parts of the gastrointestinal system, where bacteria dwell even in a healthy state).
There are multiple safeguards along the path of the respiratory system. These are designed to keep serious, pathogenic organisms from invading, and leading to infection.
The first line of defense includes the hair in the nostrils, which serves as a filter for larger particles. The epiglottis is a trap door of sorts, designed to prevent food and other swallowed substances from entering the larynx and then trachea. Sneezing and coughing, both provoked by the presence of irritants within the respiratory system, help to clear such irritants from the respiratory tract.
Mucus produced by the respiratory system also serves to trap dust and infectious organisms. Tiny hairlike projections (cilia) from cells lining the respiratory tract beat constantly. They move debris trapped by mucus upwards and out of the respiratory tract. This mechanism of protection is referred to as the mucociliary escalator.
Cells lining the respiratory tract produce several types of immune substances that protect against various organisms. Other cells (called macrophages) along the respiratory tract actually ingest and kill invading organisms.
The organisms that cause pneumonia, then, are usually carefully kept from entering the lungs by virtue of these host defenses. However, when an individual encounters a large number of organisms at once, the usual defenses may be overwhelmed. Infection may happen either by inhaling contaminated air droplets, or by aspiration of organisms inhabiting the upper airways.
CONDITIONS PREDISPOSING TO PNEUMONIA. In addition to exposure to sufficient quantities of causative organisms, certain conditions may make an individual more likely to become ill with pneumonia. Certainly, the lack of normal anatomical structure could result in an increased risk of pneumonia.
For example, there are certain inherited defects of cilia which result in less effective protection. Cigarette smoke, inhaled directly by a smoker or second-hand by an innocent bystander, interferes significantly with ciliary function, as well as inhibiting macrophage function.
Stroke, seizures, alcohol, and various drugs interfere with the function of the epiglottis. A weak epiglottis leads to a leaky seal on the trap door, with possible contamination by swallowed substances and/or regurgitated stomach contents.
Alcohol and drugs also interfere with the normal cough reflex. This inteference further decreases the chance of clearing unwanted debris from the respiratory tract.
Viruses may interfere with ciliary function, allowing themselves or other microorganism invaders (such as bacteria) access to the lower respiratory tract. One of the most important viruses is HIV (Human Immunodeficiency Virus), the causative virus in AIDS (acquired immunodeficiency syndrome). In recent years this virus has resulted in a huge increase in the incidence of pneumonia.
Because AIDS results in a general decreased effectiveness of many aspects of the host’s immune system, a patient with AIDS is susceptible to all kinds of pneumonia. This includes some previously rare parasitic types that would be unable to cause illness in an individual possessing a normal immune system.
The elderly have a less effective mucociliary escalator, as well as changes in their immune system. This causes this age group to be more at risk for the development of pneumonia.
Various chronic conditions predispose a person to infection with pneumonia. These include asthma, cystic fibrosis, and neuromuscular diseases that may interfere with the seal of the epiglottis. Esophageal disorders may result in stomach contents passing upwards into the esophagus.
This increases the risk of aspiration into the lungs of those stomach contents with their resident bacteria. Diabetes, sickle cell anemia, lymphoma, leukemia, and emphysema also predispose a person to pneumonia.
Genetic factors also appear to be involved in susceptibility to pneumonia. Certain changes in DNA appear to affect some patients’ risk of developing such complications of pneumonia as septic shock.
Pneumonia is also one of the most frequent infectious complications of all types of surgery. Many drugs used during and after surgery may increase the risk of aspiration, impair the cough reflex, and cause a patient to underfill their lungs with air. Pain after surgery also discourages a patient from breathing deeply enough, and from coughing effectively.
Radiation treatment for breast cancer increases the risk of pneumonia in some patients by weakening lung tissue.
In addition, the use of mechanical ventilators to assist patients in breathing after surgery increases their risk of developing pneumonia. The mortality rate among ventilated patients who develop pneumonia is 46%.
Causes and symptoms
Causes
The list of organisms that can cause pneumonia is very large, and includes nearly every class of infectious organism: viruses, bacteria, bacteria-like organisms, fungi, and parasites (including certain worms). Different organisms are more frequently encountered by different age groups.
Further, other characteristics of an individual may place him or her at greater risk for infection by particular types of organisms:
- Viruses cause the majority of pneumonias in young children (especially respiratory syncytial virus, parainfluenza and influenza viruses, and adenovirus).
- Adults are more frequently infected with bacteria (such as Streptococcus pneumoniae, Haemophilus influenzae, and Staphylococcus aureus).
- Pneumonia in older children and young adults is often caused by the bacteria-like Mycoplasma pneumoniae (the cause of what is often referred to as "walking" pneumonia).
- Pneumocystis carinii is an extremely important cause of pneumonia in patients with immune problems, such as patients being treated for cancer with chemotherapy, or patients with AIDS. Classically considered a parasite, it appears to be more related to fungi.
- People who have reason to come into contact with bird droppings, such as poultry workers, are at risk for pneumonia caused by the organism Chlamydia psittaci.
- A very large, serious outbreak of pneumonia occurred in 1976, when many people attending an American Legion convention were infected by a previously unknown organism. Subsequently named Legionella pneumophila, it causes what is now called “Legionnaire’s Disease.” The organism was traced to air conditioning units in the convention’s hotel.
Symptoms
Pneumonia is suspected in any patient who has fever, cough, chest pain, shortness of breath, and increased respirations (number of breaths per minute). Fever with a shaking chill is even more suspicious. Many patients cough up clumps of sputum, commonly known as spit.
These secretions are produced in the alveoli during an infection or other inflammatory condition. They may appear streaked with pus or blood. Severe pneumonia results in the signs of oxygen deprivation. This includes blue appearance of the nail beds or lips (cyanosis).
The invading organism causes symptoms, in part, by provoking an overly strong immune response in the lungs. In other words, the immune system that should help fight off infections, kicks into such high gear, that it damages the lung tissue and makes it more susceptible to infection. The small blood vessels in the lungs (capillaries) become leaky, and protein-rich fluid seeps into the alveoli.
This results in less functional area for oxygencarbon dioxide exchange. The patient becomes relatively oxygen deprived, while retaining potentially damaging carbon dioxide. The patient breathes faster and faster, in an effort to bring in more oxygen and blow off more carbon dioxide.
Mucus production is increased, and the leaky capillaries may tinge the mucus with blood. Mucus plugs actually further decrease the efficiency of gas exchange in the lung. The alveoli fill further with fluid and debris from the large number of white blood cells being produced to fight the infection.
Consolidation, a feature of bacterial pneumonias, occurs when the alveoli, which are normally hollow air spaces within the lung, instead become solid, due to quantities of fluid and debris.
Viral pneumonias and mycoplasma pneumonias do not result in consolidation. These types of pneumonia primarily infect the walls of the alveoli and the parenchyma of the lung.
Severe acute respiratory syndrome (SARS)
Severe acute respiratory syndrome, or SARS, is a contagious and potentially fatal disease that first appeared in the form of a multi-country outbreak in early February 2003.
Later that month, the CDC began to work with the World Health Organization (WHO) to investigate the cause(s) of SARS and to develop guidelines for infection control. SARS has been described as an “atypical pneumonia of unknown etiology;” by the end of March 2003, the disease agent was identified as a previously unknown coronavirus.
The early symptoms of SARS include a high fever with chills, headache, muscle cramps, and weakness. This early phase is followed by respiratory symptoms, usually a dry cough and painful or difficult breathing. Some patients require mechanical ventilation. The mortality rate of SARS is thought to be about 3%.
As of the end of March 2003, the CDC did not have clearly defined recommendations for treating SARS. Treatments that have been used include antibiotics known to be effective against bacterial pneumonia; ribavirin and other antiviral drugs; and steroids.
Diagnosis
For the most part, diagnosis is based on the patient’s report of symptoms, combined with examination of the chest. Listening with a stethoscope will reveal abnormal sounds, and tapping on the patient’s back (which should yield a resonant sound due to air filling the alveoli) may instead yield a dull thump if the alveoli are filled with fluid and debris.
Laboratory diagnosis can be made of some bacterial pneumonias by staining sputum with special chemicals and looking at it under a microscope. Identification of the specific type of bacteria may require culturing the sputum (using the sputum sample to grow greater numbers of the bacteria in a lab dish).
X-ray examination of the chest may reveal certain abnormal changes associated with pneumonia. Localized shadows obscuring areas of the lung may indicate a bacterial pneumonia, while streaky or patchy appearing changes in the x-ray picture may indicate viral or mycoplasma pneumonia. These changes on x ray, however, are known to lag in time behind the patient’s actual symptoms.
Treatment
Pneumonia is a potentially serious condition that requires prompt medical attention. Patients should contact their doctors for immediate diagnosis and treatment. Alternative treatment such as nutritional support, however, can help alleviate some of the symptoms associated with pneumonia and boost the body’s immune function.
Diet and nutrition
The following nutritional changes are recommended:
- Avoid all potentially allergenic foods, and determine allergenic foods with an elimination diet.
- Reduce intake of sugar and processed foods.
- Give yourself plenty of rest.
- Get plenty of fluids to prevent dehydration and help loosen phlegm.
- Nutritional supplements such as vitamin C, bioflavonoids, vitamin A, beta-carotene, and zinc may help.
Herbal treatment
Over-the-counter herbal preparations such as glycerol guaiacolate can help clear the lungs of phlegm and speed up the recovery process. Antimicrobial herbs, such as goldenseal (Hydrastis canadenis) and Chinese herbs, which stimulate the immune system, may be taken for treatment.
Other treatment
Other treatments, such as yoga, help with breathing, movement, and relaxation. Also recommended is meditation and the use of guided imagery. Contact local practitioners to enroll in such therapies.
Allopathic treatment
Prior to the discovery of penicillin antibiotics, bacterial pneumonia was almost always fatal. Today, antibiotics, especially given early in the course of the disease, are very effective against bacterial causes of pneumonia.
Erythromycin and tetracycline improve recovery time for symptoms of mycoplasma pneumonia. They do not, however, eradicate the organisms. Amantadine and acyclovir may be helpful against certain viral pneumonias.
A newer antibiotic named linezolid (Zyvox) is being used to treat penicillin-resistant organisms that cause pneumonia. Linezolid is the first of a new line of antibiotics known as oxazolidinones. Another new drug known as ertapenem (Invanz) is reported to be effective in treating bacterial pneumonia.
Expected results
Rate of recovery varies according to the type of organism causing the infection. Recovery following pneumonia with Mycoplasma pneumoniae is nearly 100%. Staphylococcus pneumoniae has a death rate of 30–40%.
Similarly, infections with a number of gram negative bacteria (such as those in the gastrointestinal tract which can cause infection following aspiration) have a high death rate of 25–50%.
Streptococcus pneumoniae, the most common organism causing pneumonia, produces a death rate of about 5%. More complications occur invery young or very old individuals who have multiple areas of the lung infected simultaneously.
Individuals with other chronic illnesses (including cirrhosis of the liver, congestive heart failure, individuals without a functioning spleen, and individuals who have other diseases that result in a weakened immune system) experience complications. Patients with immune disorders, various types of cancer, transplant patients, and AIDS patients also experience complications.
Prevention
Because many bacterial pneumonias occur in patients who are first infected with the influenza virus, yearly vaccination against influenza can decrease the risk of pneumonia for the elderly and people with chronic diseases such as asthma, cystic fibrosis, diabetes, kidney disease and cancer.
Maintaining a healthy diet that includes whole foods and vitamin C and B-complex vitamins will aid in prevention. Also helpful in terms of both good health and prevention of pneumonia is developing a regular exercise regimen, as well as reducing stress.
A specific vaccine against Streptococcus pneumoniae is very protective, and should also be administered to patients with chronic illnesses.
Patients who have decreased immune resistance are at higher risk for infection with Pneumocystis carinii. They are frequently put on a regular drug regimen of Trimethoprim sulfa and/or inhaled pentamidine to avoid Pneumocystis pneumonia.
